A brief history
In 1967, just 19 years after its founding, the World Health Organization (WHO) embarked on an ambitious mission to eradicate smallpox, launching a public health campaign unlike any before it. However, these plans faced unexpected complications with the discovery of monkeypox virus (now known as MPXV, the virus that causes the recently renamed disease, mpox) at the State Serum Institute in Denmark in 1958. Closely related to smallpox, MPXV raised concerns that it could hinder the global effort to eradicate smallpox. Over the next decade, the WHO conducted extensive field studies to identify potential animal reservoirs of mpox, which suggested that rodents, rather than monkeys, are likely the primary hosts. However, it wasn’t until September 1,1970, that the first human case of mpox was identified in the Democratic Republic of Congo (DRC).
For the next 50 years, mpox remained largely confined to small, sporadic outbreaks in central and western Africa. These outbreaks were typically triggered by spillover events – when the virus jumped from an animal host to a human, followed by limited human-to-human transmission among close contacts. There were some instances of outbreaks outside these regions, primarily through travel or exposure to imported and infectious wildlife.
Two clades of mpox circulate in endemic regions: Clade I and Clade II. Clades can be thought of as cousins—closely related, but with distinct traits and outcomes. Clade I is typically associated with more severe illness and higher mortality rates, with some outbreaks having a mortality rate as high as 10 percent. Clade II tends to cause milder disease. Both clades cause mpox, a disease that can result in painful and debilitating lesions, and in a smaller proportion of cases, severe lymphadenopathy (painful swelling of the lymph nodes).
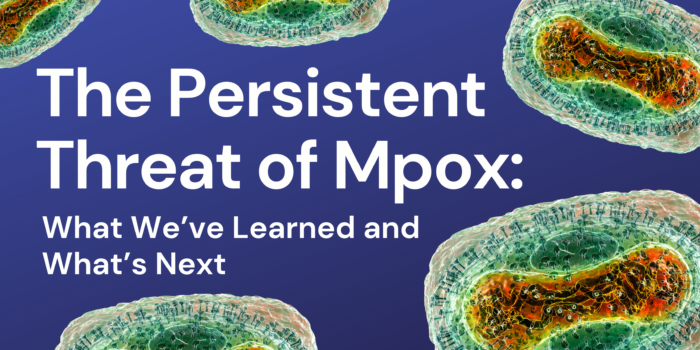
In May 2022, the global landscape and epidemiology of mpox shifted. Several countries in western Europe and North America, with no prior history of mpox transmission, began reporting cases. Over the following two months, the outbreak rapidly spread across almost every continent, with over 7,000 confirmed cases. What was equally surprising was that a majority of known transmissions were through sexual or close intimate contacts, and primarily affected gay, bisexual, and other men who have sex with men aged 18-44 years old. Previous outbreaks were primarily driven by spillover events with little evidence for sustained, human-to-human transmission.
Edouard Mathieu, Fiona Spooner, Saloni Dattani, Hannah Ritchie and Max Roser (2022) – “Mpox” Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/mpox’ [Online Resource] August 16, 2024.
Edouard Mathieu, Fiona Spooner, Saloni Dattani, Hannah Ritchie and Max Roser (2022) – “Mpox” Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/mpox’ [Online Resource] August 16, 2024.
What is driving the continued transmission of mpox?
In a forthcoming paper currently under peer review, we used simulation modeling to better understand ongoing mpox transmission dynamics that could explain the virus’s long-term persistence. We hypothesized that one or more of the following factors could be contributing to long-term persistence:
- underdetection of cases;
- waning protection from vaccination; and/or
- waning protection from infection.
To test these hypotheses, we refined an existing agent-based model of mpox, originally published by the CDC, to address our specific research questions. An agent-based model simulates individual people with specific characteristics, such as vaccination status, disease status, and propensity to form sexual partnerships. We’re simulating the spread of mpox among a representative sample of 10,000 people in the United States who are highly susceptible to the virus.
In our model, we also included various types of sexual partnerships – long-term, casual, and one-time encounters – as sexual contact was deemed a key transmission route in the 2022 outbreak. We then calibrated the model to ensure it could accurately recreate the initial outbreak, a process that allows us to root our simulations in reality.
Given the complexity of simulating outbreaks and sexual networks on a national scale, we focused on three U.S. cities: Chicago, New York, and San Francisco. We then ran 1,000 simulations for each of the hypotheses in each city to account for the inherent randomness in our models (for example, individual contacts being made). Our preliminary findings suggest that a combination of underdetection and waning immunity best explains the virus’s persistence.
What are the implications for those at risk?
Underdetection is a broad category that could include cases with very mild symptoms, asymptomatic but infectious individuals, or those who avoid seeking healthcare due to stigma but continue engaging in behaviors that could spread the virus. In our model, undetected cases remain infectious for up to 27 days, compared to just 8 days for detected cases who seek healthcare and limit further transmission. This highlights the importance of continued surveillance among at-risk populations, possibly including routine mpox screening even when there is no apparent exposure. Though the cost-effectiveness of these recommendations would need to be assessed. Underdetection of cases, especially those driven by very mild or asymptomatic cases could make it challenging to eliminate mpox completely from the United States.
Waning immunity is another crucial factor. While we know that smallpox infection typically confers lifelong protection, the duration of immunity following mpox infection is less clear. Our simulations suggest that protection may last only 12-18 months. Recent observations have documented reinfections among individuals who contracted mpox during the 2022 outbreak, but more research is needed to understand how widespread this is. The key takeaway is that those who have previously been infected with mpox should continue to take precautions and not assume they are immune to reinfection. This recommendation is similar to the guidance many are familiar with from COVID-19.
A Familiar Threat Remerges
The evolving history of mpox continues to become complicated with the re-declaration by WHO of mpox as PHEIC, given a new and rapidly growing outbreak of mpox in the DRC. This was just days after the Africa CDC had declared a Public Health Emergency of Continental Security (PHECS) over the same outbreak. However, this outbreak is somewhat different than the one we faced globally in 2022. Over the last year, the DRC has had a growing outbreak, which revealed the co-circulation of two clades of mpox. The 2022 outbreak was primarily driven by Clade II, while the emerging outbreak is primarily driven by the more deadly Clade I. Furthermore, the clades can have variants, much like COVID-19, in which a new variant was identified and believed to have emerged late last year. While the effects of these variants on health outcomes remain unknown, some researchers/medical professionals believe that some diagnostic methods are unable to detect this specific variant.
The committee determining whether to declare mpox a PHEIC was especially alarmed by the rapid dispersal of cases to neighboring countries on the continent, especially in countries that have never seen large mpox outbreaks. Unlike the 2022 outbreak, this growing outbreak is being spread both by close intimate contacts (for example, sexually) as well as close household contacts. Therefore, the demographics of those affected has also shifted from the previous outbreak, and children and women are also being infected. A majority of mpox-associated deaths in the DRC are currently among children. More recently, cases have been detected in other countries outside of Africa, though for now they are believed to be driven by travel with no suspected community transmission.
Rasalina Willamson